Tonsillectomy is specified for individuals who have
experienced more than 6 episodes of streptococcal pharyngitis (confirmed by
positive culture) in 1 year 5 episodes in 2 consecutive years or 3 or more
infections during 3 years in a row, or chronic tonsillitis or recurrent related
state of carrier of streptococcus that did not respond to antibiotics resistant
to beta-lactamase. Tonsillectomy can result in children when multiple
allergies or antibiotic intolerance are observed, as well as children with
periodic fever, pharyngitis and adenitis (PFAPA), aphthous or peritonsillar
history . Since the adenoid tissue has a comparative bacteriology with
pharyngeal tonsils and due to the fact that adenoidectomy an insignificant and
singularity occurs if a tonsillectomy as now is done, most specialists perform
an adenoidectomy if adenoids are available and illuminated at the time of
tonsillectomy. In any case, this point remains doubtful. Intermittent
tonsillitis after tonsillectomy is very rare. Tonsillectomy decreases bacteria
sack of Streptococcus pyogenes hemolytic collection (GABHS) and may also allow
expansion of alpha-streptococci, which can be defense against GABHS disease.
Intermittent tonsillitis is usually due to the re-growth of tonsillar tissue,
which is treated by extraction. Tonsillectomy with or without adenoidectomy is
the treatment for endless tonsillitis. In cases of special infinite tonsillitis
for specialized tonsillectomy contemplations include awareness of greater
intraoperative and perioperative drainage, and the awareness that the
dismemberment may be more problematic in light of fibrosis and scarring of the
tonsil container.
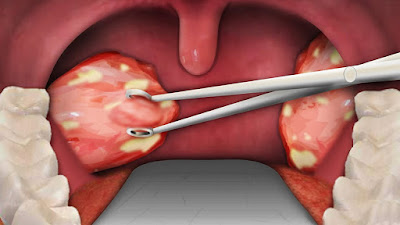 |
| Tonsillectomy |
A study by Wang et al specified that
tonsillectomy increases the risk of deep-neck contamination. Using a search in
the health insurance research database, the researchers found that patients had
a 1.75-fold increased risk of deep-neck infection after undergoing
tonsillectomy. A retrospective cohort study on 61,430 patients undergoing
tonsillectomy specifies that the use of intravenous steroids on the day of
surgery increases the frequency of post-tonsilectomía bleeding in children but
not in adults. In the study, Suzuki et al. Found that the reoperation rate for bleeding was 1.2% for children aged 15 or less who received intravenous steroids, versus 0.5% for patients in the same age group who have not. Among patients over the age of 15 however, the reoperation rate was not significantly higher in steroid patients than in controls (1.7% vs 1.4%) .
A review of the literature of De Luca Canto et al
showed that the compromise is the maximum Frequent
complications in children (9.4%) after adenotonsillectomy, secondary
haemorrhage is the second most frequent (2.6%). The authors also found that children who experience
adenotonsillectomy, the risk of respiratory complications is 4.9 times higher
in patients with obstructive sleep apnea in children who do not, but the risk
of postoperative bleeding is lower .
A retrospective study by Spektor et al points out
that the risk of postoperative bleeding in children undergoing tonsillectomy
expands when surgery is performed in a child with recurrent tonsillitis
(4.5-fold risk) in a child with a deficiency of responsiveness. Hyperactivity disorder (8.7 times higher
risk), or in an older child (twice the risk of bleeding in children 11 years
and older).







0 comments:
Post a Comment